Updates from America — Part 1 of 4
1. Since 2 Oct 2020, the number of Americans infected has been growing at an exponential rate. Even the US President Donald Trump and the first lady, Melania Trump have tested positive for COVID-19 on that day.
4. Biden’s first major announcement after being projected the winner of the election, was to announce a coronavirus advisory board to guide him during the transition.
5. The task force is chaired by former Surgeon General Vivek Murthy, former Food and Drug Administration commissioner David Kessler and Yale University's Dr. Marcella Nunez-Smith. Among the other members are Dr. Luciana Borio, a senior fellow for global health at the Council on Foreign Relations, and Dr. Zeke Emanuel, one of the architects of the Affordable Care Act and an ex-Obama health adviser. The latest announcement of Biden's selection of:
1. Since 2 Oct 2020, the number of Americans infected has been growing at an exponential rate. Even the US President Donald Trump and the first lady, Melania Trump have tested positive for COVID-19 on that day.
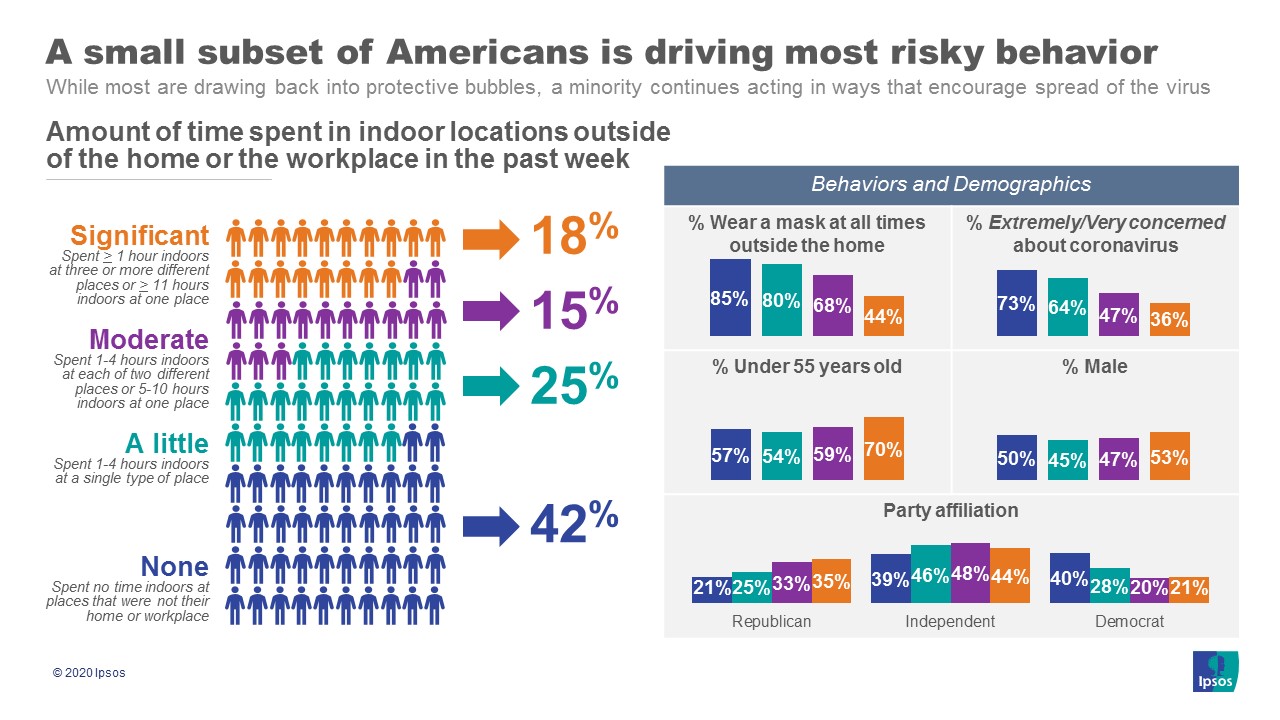
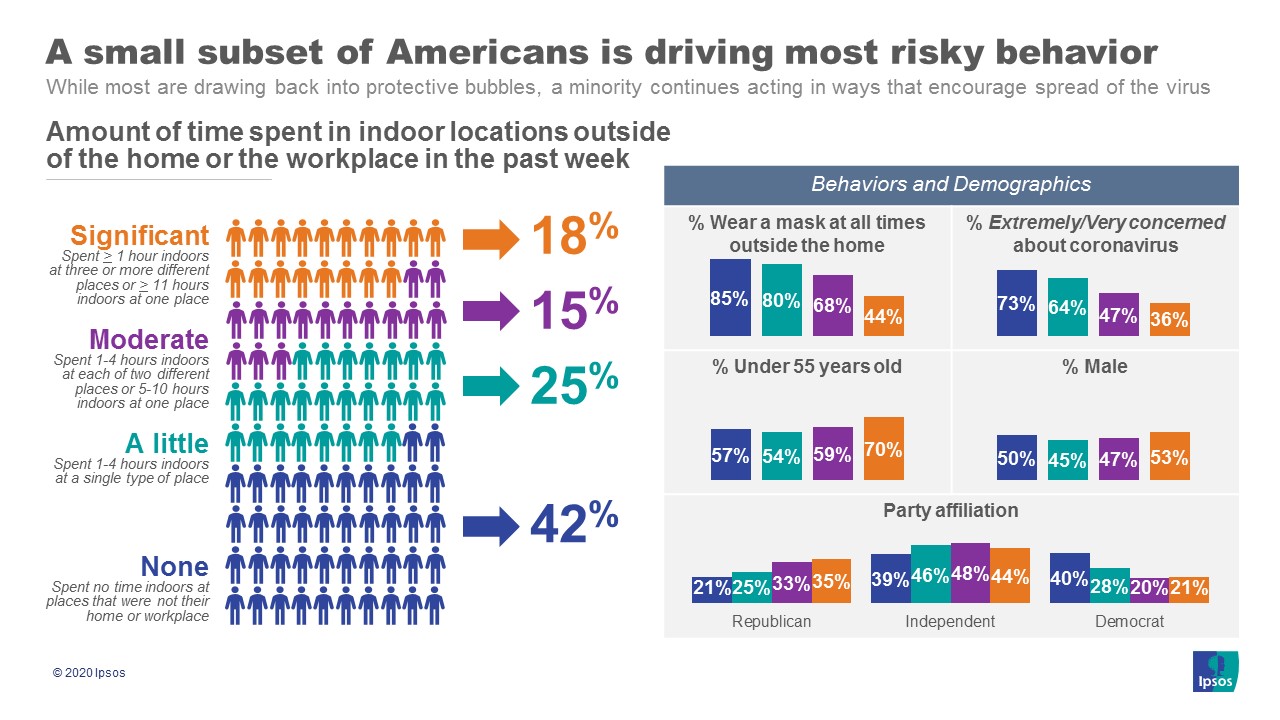
(a) As daily deaths from the coronavirus reach new records, a new IPSOS/Axios poll finds that a core group of 18% of Americans, like Trump, continue to regularly engage in the behaviors thought riskiest for spreading the disease.
- This group spent at least an hour restaurants & bars, entertainment centers, other people’s homes, gyms, or places of worship; or spent over 10 hours total indoors out of home in the last week.
- 44% of this group report wearing a mask at all times and only 36% are concerned about the coronavirus pandemic.
- This group tends to be under the age of 55, more likely to be male, and more likely to be Republican.
- People who primarily get their news from local sources or do not consume news are more likely to be in this group.
(b) The rest of Americans are more worried about the coronavirus now than at any point since early this Summer.
- 60% of Americans are extremely or very concerned about the coronavirus outbreak with an additional 25% somewhat concerned. This high level has sustained from before Thanksgiving and was last seen in June.
- Almost 73% say returning to a pre-coronavirus life right now would be a large or moderate risk, the highest levels seen since this question began tracking in April.
(c) Interest in the first generation COVID-19 vaccine continues to climb as it becomes more of a reality.
- This week, over 53% say they would be likely to get the first generation COVID-19 vaccine as soon as it is available, up from 51% before Thanksgiving and 38% in early October.
- Most people are more likely to take a COVID-19 vaccine if it
- has been proven safe and effective by public health officials (69%),
- has a 90%+ effectiveness rate (67%), or
- has been on the market a few months (65%).
- When presented with a situation where former presidents Obama, Bush, and Clinton take the vaccine publicly, 60% say they would be likely to take it. An improvement over the baseline but not as convincing as the safety arguments.
- 3,054 deaths;
- 209,822 new coronavirus cases; and
- 106,688 hospitalizations.
4. Biden’s first major announcement after being projected the winner of the election, was to announce a coronavirus advisory board to guide him during the transition.
5. The task force is chaired by former Surgeon General Vivek Murthy, former Food and Drug Administration commissioner David Kessler and Yale University's Dr. Marcella Nunez-Smith. Among the other members are Dr. Luciana Borio, a senior fellow for global health at the Council on Foreign Relations, and Dr. Zeke Emanuel, one of the architects of the Affordable Care Act and an ex-Obama health adviser. The latest announcement of Biden's selection of:
(a) infectious disease expert Dr. Rochelle Walensky to head the CDC; The CDC will manage the distribution of a Covid vaccine, a complex process that will be one of the largest immunization campaigns in U.S. history. Health care leaders celebrated Walensky’s appointment after the news broke.
(b) Xavier Becerra as Health Secretary (Attorney General of California and former member of the House of Representatives);
(c) the return of Dr. Vivek Murthy as surgeon general;
(d) the elevation of Dr. Anthony Fauci to medical adviser;
(e) Dr. Marcella Nunez-Smith as a COVID-19 Equity Task Force chair (Nunez-Smith is an Associate Professor of Medicine, Public Health, and Management at the Yale School of Medicine);
(f) Jeff Zients as Coronavirus Coordinator (Zients previously earned broad acclaim for his leadership of the 2013 HealthCare.gov tech surge and his oversight of the ‘Cash for Clunkers’ fuel-efficiency program); and
(g) Natalie Quillian as Deputy Coordinator of the COVID-19 Response (Quillian is a national security expert, former White House and Pentagon senior advisor, who had played an instrumental role in coordinating the Obama-Biden administration’s interagency response to the opioid epidemic),
all point to a more assertive federal coronavirus role and a restoration of the traditionally important role of science in public health emergencies.
Last edited:

